PATHOLOGIES
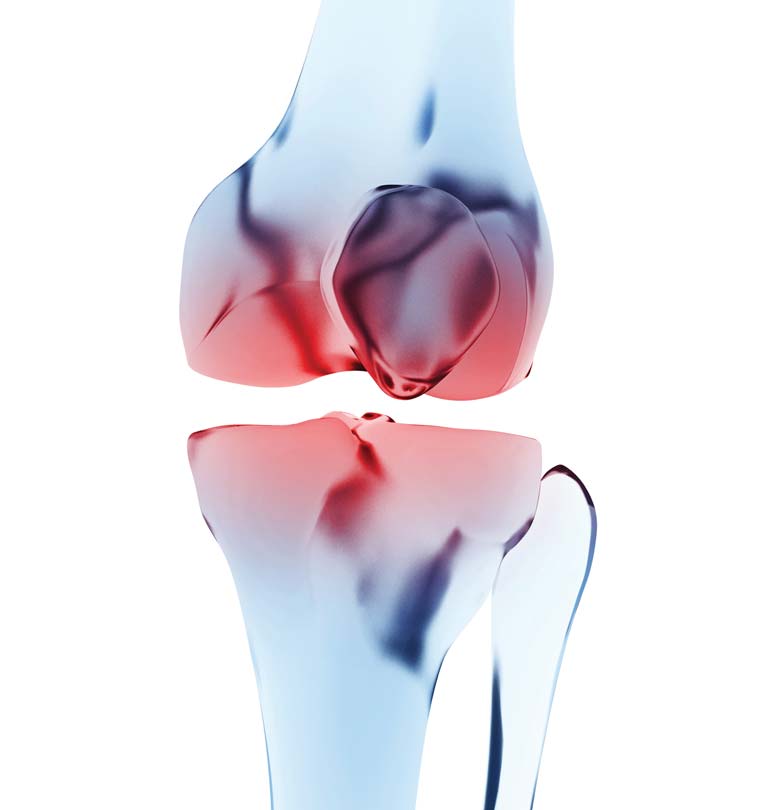
Gonarthrosis
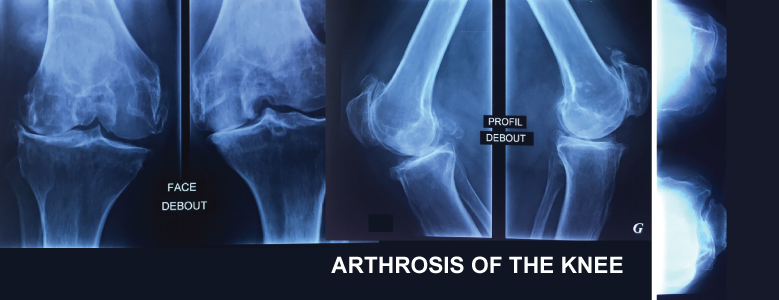
Knee osteoarthritis is a gradual wear of the joint cartilaginous surface of the knee. This gradually leads to a painful knee disability. This pathology slightly more frequently affects women .Some risk factors are found: heredity, deformities or misalignment of the lower limbs, obesity, rheumatic diseases, trauma background: fractures, ligament injuries and or meniscal.
DIAGNOSTIC
- Pain: main symptom: persistent, progressing by thrust at the beginning, of variable intensity becoming unbearable during crises, increasing during prolonged efforts.
- Stiffness: limitation of motion is seen in advanced osteoarthritis
- Important effusions concurrent with thrusts, increasing pain which causes functional impairment.
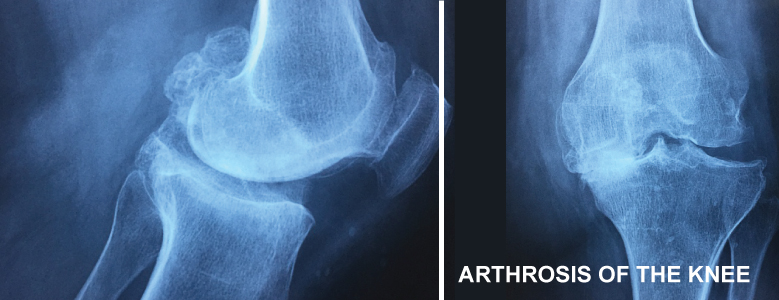
- Complementary examinations:
- Initial check-up: Simple radiographs: are often sufficient, should be carried out(standing patients)in charge, to assess the importance of the joint space narrowing and the evolution of osteoarthritis stage.
- Telemetric radiographs: allow to calculate the axial deviation of the lower limbs.
- MRI: important in case of osteoarthritis which are in their first phase and which also are rebelling against medical treatment with a strong suspicion of painful meniscal lesion.
TREATMENT
- Medical: MEDICAL: analgesics, anti-inflammatories ,infiltrations and rehabilitation are used for beginning phases and can relieve pain without stopping osteoarthritis development.
- Surgical: The decision and choice the surgery type depends on the importance of osteoarthritis, discomfort felt by the patient and his will, his age and general health condition. Two major types of interventions are performed:
- Conservative treatment:
- Arthroscopy: in case of unstable meniscal lesions in the beginning of osteoarthritis
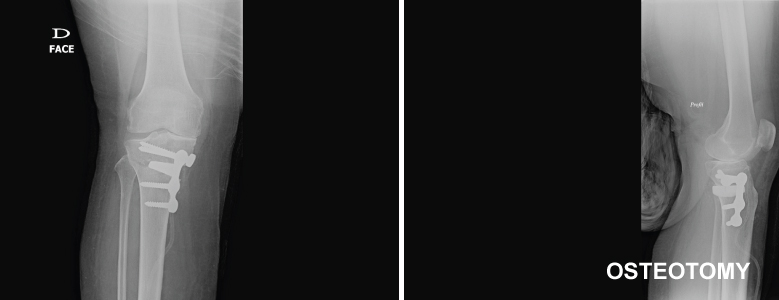
- Tibial osteotomy: this intervention is performed to correct bone deformities responsible for a pinch at the knee compartment. This bony correction is maintained by installing screwed plates. New generations of plates allow almost immediate support unlike the former which are less expensive but prohibit the support for 6 and 8 weeks.
We use only the new generation of plates, so we systematically refuse to make this intervention with the older generation just to reduce costs.
- Prosthetic surgery: two types of prostheses can be put:
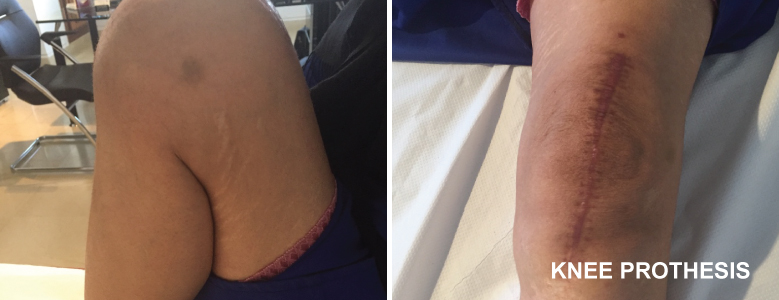
- Total knee prosthesis: the most frequent: is intended for advanced stages of osteoarthritis or osteoarthritis affecting all knee compartments. The age of the prosthesis implantation is delayed as much as possible without expecting a limitation of the patients autonomy. This operation is quite heavy on the anesthetic level (painful postoperative and significant blood loss). It must therefore be rigorously well prepared and followed to ensure the best results with a very low complication rate.
- Uni-compartmental prosthesis: is intended for young patients having localized osteoarthritis without possibility of making an osteotomy. It is also performed for seniors whose the installation of a total prosthesis is hard to bear or whose osteoarthritis is unsophisticated but annoying.
FOLLOW-UP
Hospitalizations average is 3-7 days depending on the type of performed operation. The arthroscopy will take place in ambulatory (the patient can exit the same day) Rehabilitation is immediate, it is made easier by the installation of a loco-regional bloc of the operated limb with continuous instillation of analgesics. The motion is activo-passive from the bigginning (arthromoteur + + +). Applying immediate support for the majority of cases. Gradual Recovery with an almost normal movement between the 3rd and 5th months. The improvement can continue over a year leaving an important margin of appreciation. Recovery is faster thanks to conservative interventions. Like any prosthesis, this one has an average lifespan of 15 years. Regular follow-up is therefore necessary to act in case of necessary resumption.